Jan 7, 2026
Digital forms have become a cornerstone of modern healthcare workflows. Yet not all forms serve the same purpose. In practice, we see three distinct roles: remote monitoring, hybrid care pathways, and clinical documentation & screening. Each type supports a different moment in the care journey—and when used correctly, they significantly reduce administrative burden while improving clinical insight. In this article, we explore these three ways to deploy healthcare forms and how they complement each other within interoperable care environments.
Table: 3 commonly used healthcare forms
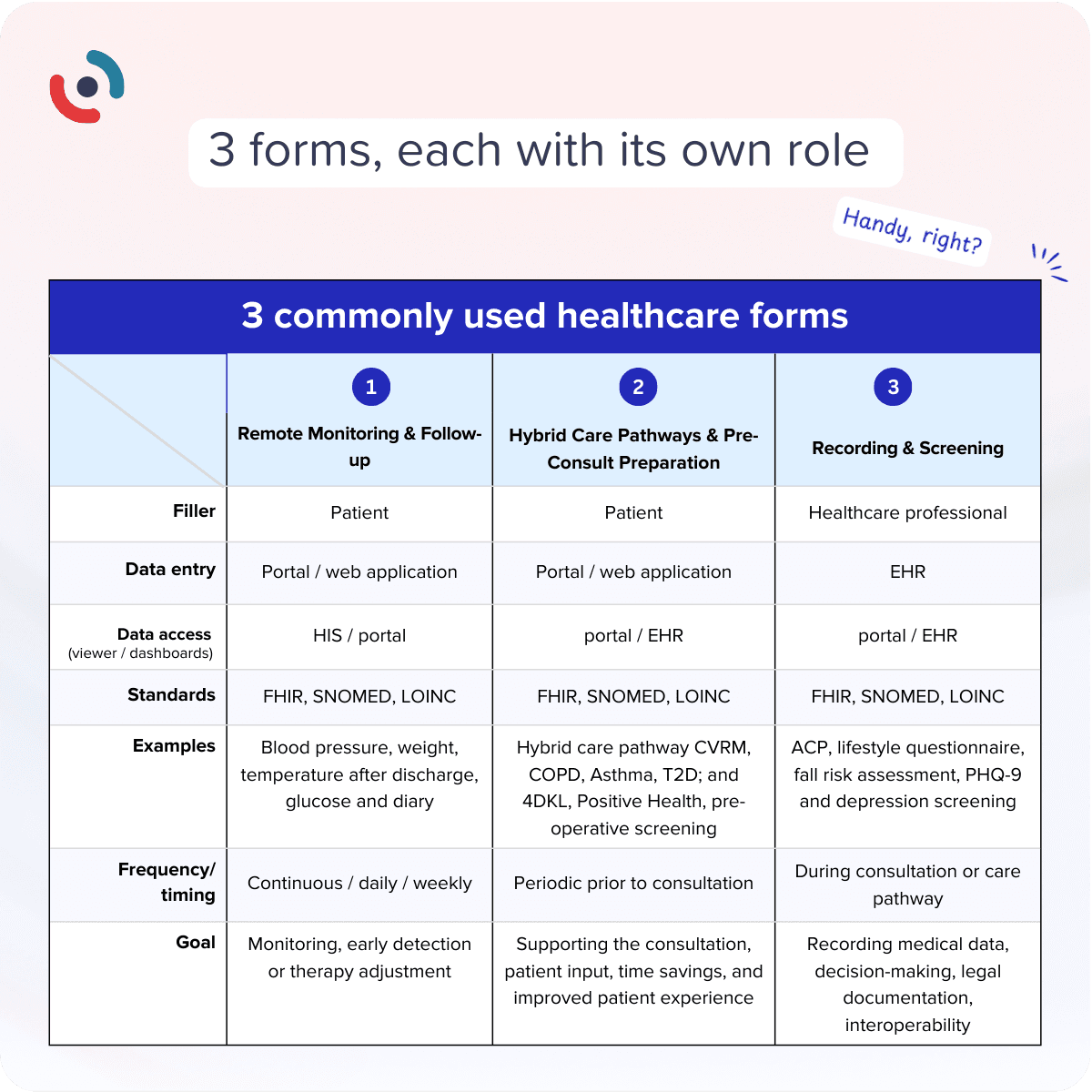
1. Remote Monitoring & Follow-up
Continuous insight into patient status between consultations
Remote monitoring forms allow patients to report measurements and symptoms from home. Think of blood pressure readings after discharge, glucose logs, or symptom diaries. These forms are typically filled in by the patient via a portal or web application and viewed by clinicians in the HIS, EHR, or care dashboards.
The key value lies in continuity. Instead of relying on a single consultation snapshot, clinicians gain a longitudinal view of the patient’s condition. This supports early detection of deterioration, proactive interventions, and therapy adjustments.
Typical characteristics:
Completed by: Patient
Timing: Continuous, daily, or weekly
Goal: Monitoring, early detection, therapy optimization
Standards: Often based on FHIR, NHG guidelines, and SNOMED terminology
Remote monitoring forms are especially valuable for chronic disease management such as CVRM, COPD, asthma, and diabetes.
2. Hybrid Care Pathways & Consultation Preparation
Better conversations through structured pre-consult input
The second category focuses on preparing and enriching consultations. Patients complete structured questionnaires before their appointment, contributing relevant information about symptoms, lifestyle, or concerns.
These forms are typically filled in periodically before a consultation and become available across systems such as patient portals, EHRs, or care coordination platforms.
The result? Consultations become more focused and meaningful. Clinicians start with context, patients feel heard, and valuable consultation time is used more efficiently.
Typical characteristics:
Completed by: Patient
Timing: Periodically, prior to consultation
Goal: Better preparation, patient input, time savings, improved patient experience
Examples include CVRM pathway questionnaires, lifestyle assessments, or positive health screenings embedded in hybrid care pathways.
3. Clinical Documentation & Screening
Structured capture of medical data for decision-making and interoperability
The third role is fundamentally different: forms completed by healthcare professionals to document findings, perform screenings, and support clinical decision-making.
These forms are usually entered directly into HIS, EHR, or ECD systems and serve as a legally relevant and interoperable record of care.
By standardizing how data is captured, organizations ensure that information is reusable across systems and accessible for reporting, analytics, and care coordination.
Typical characteristics:
Completed by: Healthcare professional
Timing: Snapshot during consultation or care episode
Goal: Medical documentation, decision support, legal record, interoperability
Common examples include advance care planning (ACP/PZP), fall risk assessments, PHQ-9 depression screening, and lifestyle questionnaires.
One Care Journey, Three Complementary Roles
Although these forms differ in purpose, they are most powerful when combined within one connected care flow:
Remote monitoring provides continuous data between visits.
Hybrid care pathway forms enrich the consultation with patient input.
Documentation & screening forms capture structured clinical decisions.
Together, they create a complete, context-rich patient record that supports better decision-making and coordinated care across the healthcare network.
Why This Matters for Interoperable Healthcare
When forms are built on standards such as FHIR and SNOMED, the captured data can seamlessly flow between patient portals, EHRs, and partner systems. This enables:
Reduced administrative burden
Better-informed clinicians
Engaged patients contributing to their own care
Reliable, reusable structured data for analytics and AI
Ultimately, structured forms are not just digital questionnaires—they are building blocks of scalable, interoperable, and patient-centered care.
Conclusion
Healthcare forms are not one-size-fits-all. Remote monitoring, hybrid care pathway questionnaires, and clinical documentation forms each serve a distinct function in the care process. Understanding these roles helps organizations deploy forms more strategically and unlock their full value in improving outcomes, efficiency, and interoperability.